Overview
Kyphoplasty and sacroplasty are procedural techniques used to address compression fractures in the spine. Sacroplasty is a rare procedure used to address fractures in the sacrum. Both kyphoplasty and sacroplasty use similar procedural techniques. Kyphoplasty is more much commonly used to treat compression fractures of the thoracic and lumbar spine. The procedure is typically outpatient and uses a large needle to access the fracture. A small space is created in the fracture and then a medical grade glue or cement is injected to help stabilize the fracture. This glue or cement is similar to what is used to hold joint replacements in place. The procedure typically reduces pain and prevents the fracture from worsening.
What conditions are treated with kyphoplasty or sacroplasty?
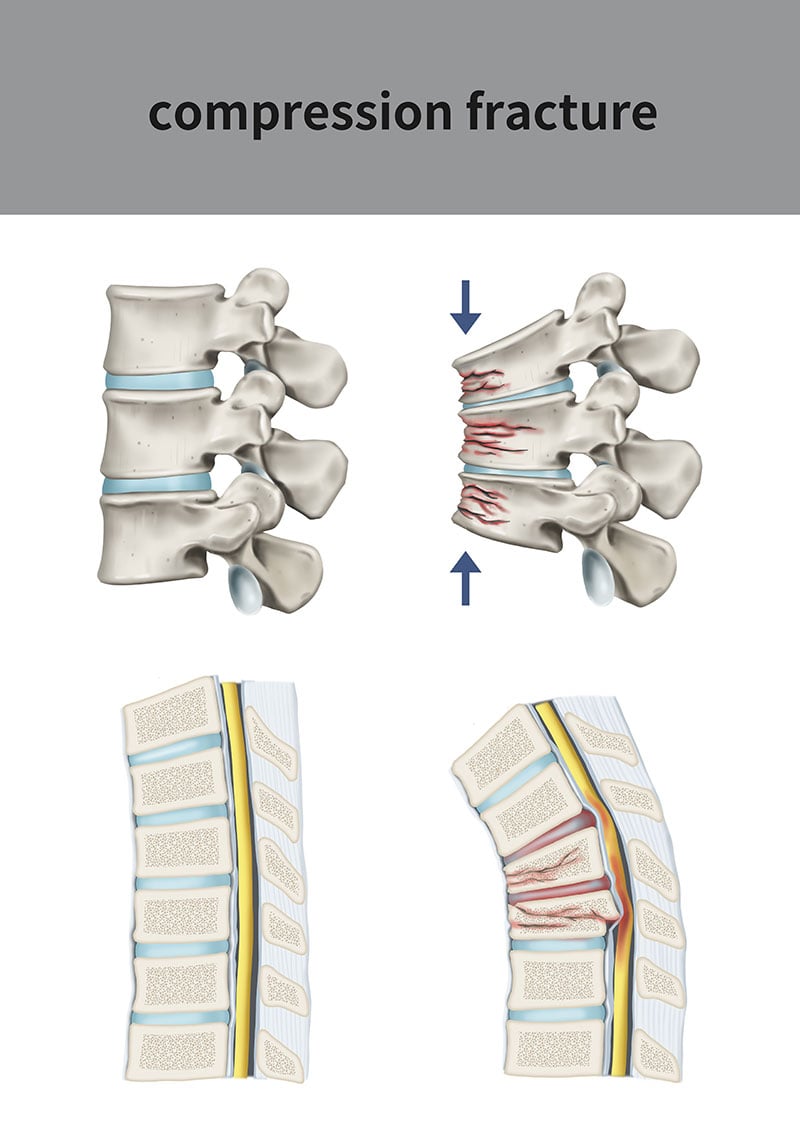
Sacroplasty and kyphoplasty are both used to treat compression fractures of the spine. Sacral fractures or sacral insufficiency is treated with sacroplasty. A vertebral compression fracture is a fracture of the vertebral body. A vertebral compression fracture is the most common type of osteoporotic fracture, and is also a very common fracture related to metastatic disease caused by cancer. Vertebral compression fractures often occur after falls or trauma such as car accidents. The vertebral body appears compressed, causing significant pain and worsened kyphosis (forward bending of the spine). Kyphoplasty is used to not only help with pain from the fracture but also decrease the chances of worsening spinal deformities.
Vertebral compression fractures are usually divided into two sub-groups, acute and chronic. MRI imaging can help determine how long a fracture has been present.
Acute fractures are recent fractures that often contribute to significant back pain. It has been shown that acute fractures can significantly impact a person’s quality of life. If left untreated, acute fractures become chronic and can lead to more debilitating problems.
Chronic fractures are much older and have typically been present for months to years. These fractures can contribute to more problematic issues such as decreased pulmonary function, GI dysfunction, hip pain and adjacent vertebral fracture risk.
How is the procedure performed?
Kyphoplasty is done in the operating room, usually under general anesthesia or with light sedation. Under fluoroscopy (x-ray), a balloon catheter is guided into the fractured vertebral body and inflated with a liquid under pressure. As the balloon inflates, it helps restore the height in the collapsed vertebral body and can correct abnormal wedging of the broken vertebra. Once maximally inflated, the balloon is then deflated and removed, thus leaving a large cavity in the vertebral body. This cavity is then filled with bone cement under low pressure, which then hardens in place, maintaining correction of the collapse and wedging.
Does the procedure hurt?
The procedure is typically well tolerated. During the procedure a pressure sensation is often experienced this typically resolves within a few minutes. Minor soreness for a week after the procedure is normal.
How long does the procedure take?
The procedure typically takes about 1 hour to perform. Please plan on being at the surgery center or hospital for about 3-4 hour to allow for pre and post-procedural safety protocols.
How quickly will I get relief?
Relief should start within 1 week.
How long can I expect the relief to last?
Every patient is different. Our goal is for you to get long-term relief.
How often can the procedure be repeated?
The procedure typically does not need to be repeated. However, if you have another area of fracture the procedure may need to be repeated at the areas.
What are the risks and side effects?
Risks and side effects are minimal and serious complications are rare. We take every precaution to ensure safety.
There is a risk of the cement leaking out of the vertebra before final hardening. If this cement leaks back into the spinal canal, it can compress the spinal cord and nerves, causing pain and neurologic problems. There are also minor risks of infection, bleeding and the possibility that the intervention may not help the patient’s pain.
As with any medical intervention, there are risks associated with the interventional procedure. Risks are present regardless of the skill, care, and experience of the physician performing the procedure. In most cases these risks and hazards are minimal and serious complications are rare.
Potential risks may include, but are not limited to: vasovagal response (passing out), new or increase of pain, infection, bleeding, permanent skin changes, allergic or unexpected drug reaction with minor or major consequences, nerve injury, paralysis, dural puncture, and headache. Procedures in the neck have the added risks of seizure, stroke, and death.
Pre-Procedure Information
Please let us know if you have an active infection, are using antibiotics, or are using blood thinners.
Should I take my normal medications as scheduled?
Yes. Continue taking your prescribed medications prior to procedure.
What if I am on a blood thinner or Aspirin?
Anticoagulation is often stopped for a short period of time prior to injection. Please speak with your primary physician if you take blood thinners to make sure that you can safely stop taking these medications.
Do I need a driver?
Yes. For your safety we require a driver to ensure a safe return home.
Can I eat the day of the procedure?
You must fast for at least 8 hours prior to the procedure. Do not eat after midnight the night before the procedure.
Can I get sedation or anesthesia?
IV anesthesia is provided. A breathing tube is typically not needed. The anesthesia level is similar to that of a colonoscopy.
What if I am pregnant?
There are serious potential risks to an unborn fetus when exposed to imaging studies, including x-ray and fluoroscopy. If there is any chance you may be pregnant, please postpone this procedure until it can be confirmed that you are not pregnant as it is not safe to do during pregnancy.
What should I wear?
We recommend light loose-fitting clothes. We will ask you to change into a gown.
Post-Procedure Information
When can I drive after the procedure?
We recommend resuming driving in about 1 week.
What can I do if I am sore or have pain after the procedure?
Ice packs can be applied to the area for 20 minutes per hour. Over the counter Tylenol and Motrin can be used to aid with any discomfort. Patients typically are sent home with pain medication.
What are my restrictions after the procedure?
Typically, you may resume light activities on the same day following your procedure. Patients resume activity as tolerated over the next 1-2 weeks.
When can I shower?
Typically we recommend no showering for 3 days. At this point the dressing can be removed and showering can be done with soap and water. Do not submerge the wound in water for 6 weeks.
When do I come back for a follow-up visit?
We follow-up with all of our patients after their procedures. We typically see patients back in 2 weeks.
