Overview
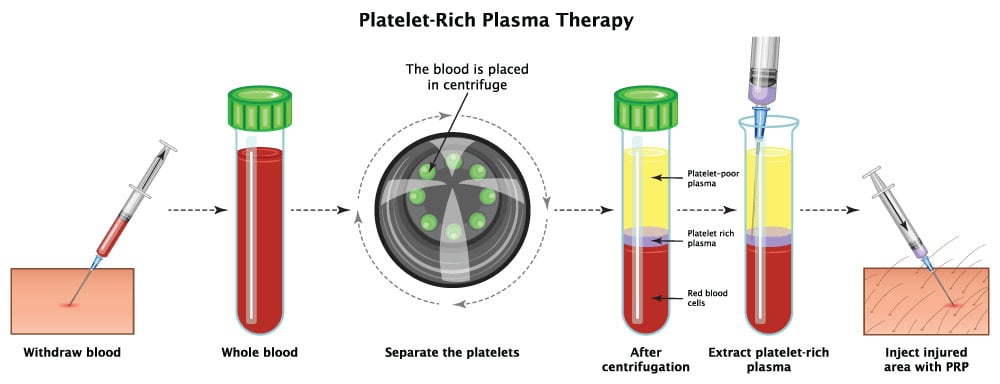
Platelet rich plasma (PRP) is a regenerative medicine therapy. This therapy first began widespread use in athletes 10-15 years ago. The injection is intended to treat a variety of arthritic joint and tendon problems. Platelet rich plasma is derived from each patient's own blood. A sample of blood is drawn when a patient arrives at the clinic. This sample is centrifuged or spun down so that the different layers are separated out. The platelet layer is identified and isolated. This platelet rich layer is rich with growth factors that accelerates the body's own healing process. The PRP is typically injected near or in the area of degeneration.
What conditions are treated with Platelet Rich Plasma Injections?
Platelet Rich Plasma (PRP) injections are used to treat a variety of tendon related injuries such as rotator cuff tendinosis, tennis elbow, and Achilles tendonitis. PRP is also used to treat joint related arthritis. Commonly treated joints include but are not limited to the hips, knees, and shoulder.
How is the procedure performed?
Our team will help position you to make sure the procedure can be completed with the least amount of discomfort for you. The skin is cleansed with a sterilizing solution (chlorhexidine) and a sterile drape is placed. A sample of blood is drawn. The blood is then centrifuged for 15-20 minutes and placed in a new sterile syringe for injection.
At the area of the intended injection site the skin is cleansed with a sterilizing solution (chlorhexidine) and a sterile drape is placed. A local anesthetic medication typically (Lidocaine) is given to numb the skin. Next the needle(s) is directed to the desired location using ultrasound or fluoroscopy (x-ray). The PRP is then injected at the target site. During the entire procedure you will be constantly monitored by the physician. After the injection a small bandage is placed on your skin. You will be given time after the procedure to make sure you feel good and are not having side-effects before leaving the clinic.
What medication is injected?
The injection includes a combination of anesthetic (lidocaine or bupivacaine) for the skin. The PRP is injected direct at the injury location.
Does the procedure hurt?
The procedure is typically well tolerated. A localized burning sensation from the anesthetic is commonly felt and is usually the most uncomfortable part of the process. During the procedure a pressure sensation is often experienced this typically resolves within a few minutes. Minor soreness for a week after the procedure is normal.
How long does the procedure take?
The procedure typically takes about 15 minutes to perform. Please plan on being at the clinic for about 1 hour to allow for pre- and post-procedural safety protocols.
How quickly will I get relief?
It can take weeks to months for the full effect of the PRP to begin the healing process. Our clinical nurse should call you on the following day to check on you. Future planned injections can be scheduled at that time.
How long can I expect the relief to last?
Every patient is different, our goal is to get long-term relief. Sometimes this requires more than one injection.
How often can the procedure be repeated?
Depending on results and providers discretion the injections may be repeated every 1-3 months. Typically, the injection is repeated two times.
What are the risks and side effects?
Risks and side effects are minimal and serious complications are rare. We take every precaution to ensure safety. Potential risks may include but are not limited to: vasovagal response (passing out), new or increased pain, infection, bleeding, permanent skin changes, allergic or unexpected drug reaction with minor or major consequences, and unintended nerve injury.
Pre-Procedure Information
Please let us know if you have an active infection, are using antibiotics, or are using blood thinners.
Should I take my normal medications as scheduled?
Yes. Continue prescribed medications as you typically take prior to procedure.
What if I am on a blood thinner or Aspirin?
Anticoagulation is often stopped for a short period of time prior to injection. Please speak with your primary physician if you take blood thinners to make sure that you can safely stop taking these medications.
Do I need a driver?
Yes. For your safety we require a driver to take you home.
Can I eat the day of the procedure?
It depends on the location. We recommend eating a light meal if the injection is done in our clinic. If the procedure is done at the surgery center, then you must fast for at least 8 hours prior to the procedure.
Can I get sedation or anesthesia?
Most patients do well without sedation. Light sedation with oral medications is sometimes provided at the physician’s discretion.
What if I am pregnant?
There are serious potential risks to an unborn fetus when exposed to imaging studies, including x-ray and fluoroscopy. If there is any chance you may be pregnant, please postpone this procedure until it can be confirmed that you are not pregnant as it is not safe to do during pregnancy.
What should I wear?
We recommend light loose-fitting clothes. Sometimes we will ask you to change into a gown.
Post-Procedure Information
When can I drive after the procedure?
We recommend resuming driving the next day.
What can I do if I am sore or have pain after the procedure?
Ice packs can be applied to the area for 20 minutes per hour. We typically ask you to refrain from using NSAIDs such as Mortin, ibuprofen, and Aleve.
What are my restrictions after the procedure?
Typically, you may resume light activities on the same day following your procedure. Physical therapy can be re-started within 24 hours. We recommend returning to work the day after the procedure.
When can I shower?
Showering the day of the procedure is allowed. For 24 hours you are asked to refrain from submerging or swimming in water. Keep the bandage on for one day.
When do I come back for a follow-up visit?
We follow-up with all of our patients after their procedures. We typically see patients back in 2-4 weeks.
